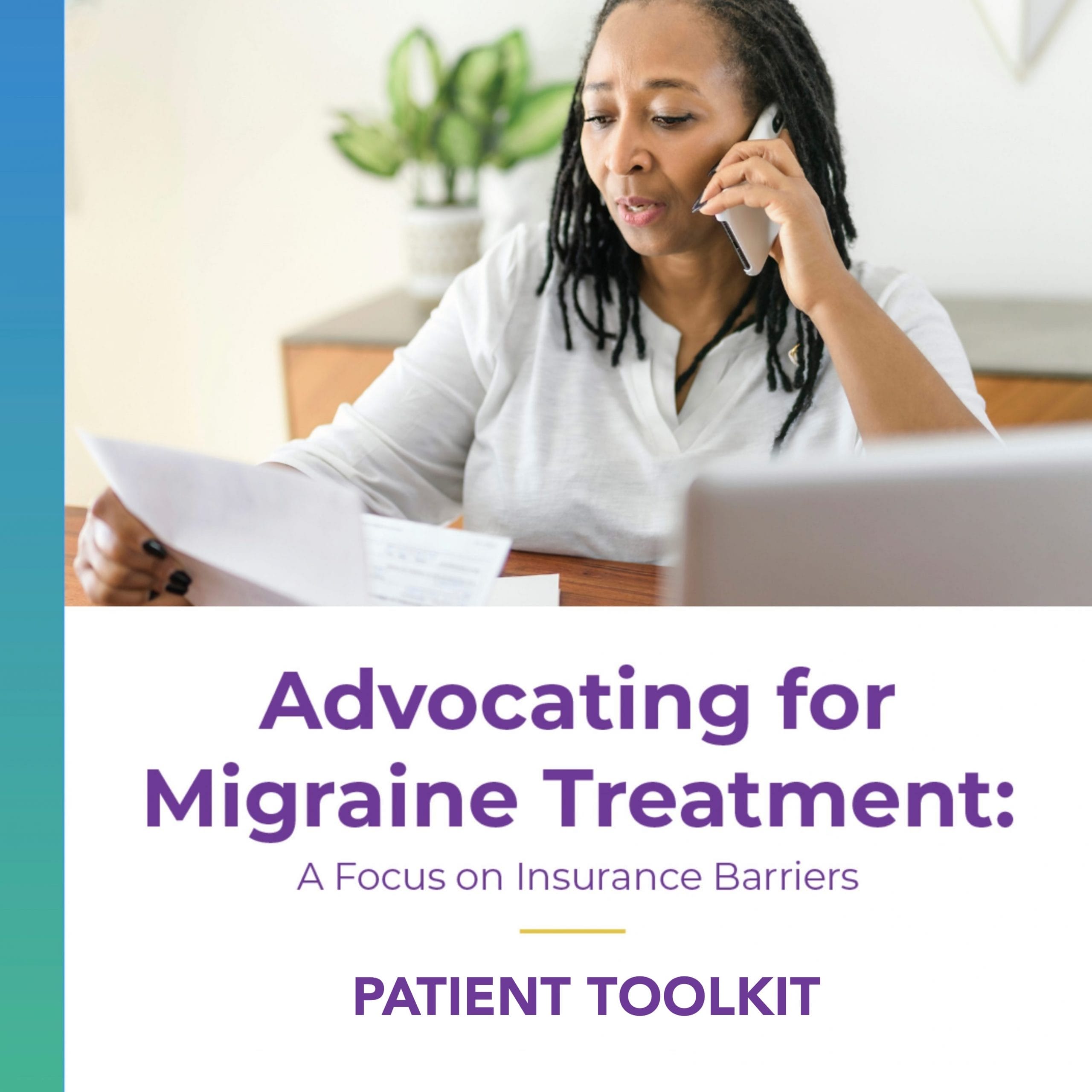
Navigating the insurance process can be overwhelming. Many of the older preventive and abortive treatments are easily available with health insurance in the USA, although some have high co-pays and are approved in limited monthly quantities. However, frequently there are access barriers put up by insurance companies. These can be challenging and time-consuming to resolve, and this is especially true for the newer migraine medications, combination therapy, and medical devices.
Insurance Terms to Know
Prior Authorization (PA)
 “Prior authorization is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.” (AMA) Many treatments require your doctor to request a PA in order for insurance to cover them. These are often treatments on your insurance company’s formulary but not accessible without additional information being required.
“Prior authorization is a health plan cost-control process by which physicians and other health care providers must obtain advance approval from a health plan before a specific service is delivered to the patient to qualify for payment coverage.” (AMA) Many treatments require your doctor to request a PA in order for insurance to cover them. These are often treatments on your insurance company’s formulary but not accessible without additional information being required.
Step Therapy
 Step therapy is when the insurer requires the patient to try one or more different medications before approving a new medication prescribed by a doctor. Most insurers have a list of medications that are preferred. Often these are less expensive and have been on the market for a while. The requirement is for patients to try the insurer-recommended medication for a specific amount of time and “fail”—meaning the patient needs to prove it is not a successful treatment before the new medication will be covered.
Step therapy is when the insurer requires the patient to try one or more different medications before approving a new medication prescribed by a doctor. Most insurers have a list of medications that are preferred. Often these are less expensive and have been on the market for a while. The requirement is for patients to try the insurer-recommended medication for a specific amount of time and “fail”—meaning the patient needs to prove it is not a successful treatment before the new medication will be covered.
Non-Medical Switching
 Non-medical switching is when an insurance company changes a patients' medication for reasons other than efficacy or side effects. Often done as a cost-savings measure, insurers may force patients to stop taking a medication that is working for them and switch to one that is less or not effective. This practice is done against the recommendations of doctors and without regard for patients' needs.
Non-medical switching is when an insurance company changes a patients' medication for reasons other than efficacy or side effects. Often done as a cost-savings measure, insurers may force patients to stop taking a medication that is working for them and switch to one that is less or not effective. This practice is done against the recommendations of doctors and without regard for patients' needs.
Combination Therapy
 Often, people with migraine need more than one prescribed treatment in their migraine toolbox, both for helping prevent migraine attacks as well as for stopping attacks that happen. Despite the success patients report with taking a combination of migraine treatments, insurance often poses barriers to accessing them. In some cases, forcing patients to choose between a preventive and an acute medication.
Often, people with migraine need more than one prescribed treatment in their migraine toolbox, both for helping prevent migraine attacks as well as for stopping attacks that happen. Despite the success patients report with taking a combination of migraine treatments, insurance often poses barriers to accessing them. In some cases, forcing patients to choose between a preventive and an acute medication.
Formulary Exception
 There are some medications that require a “Formulary Exception” request to be completed by your doctor. This is normally needed when the treatment is not listed on your insurance company’s formulary list. Your doctor has to submit additional information to show medical necessity, explaining why treatments on the formulary are not appropriate.
There are some medications that require a “Formulary Exception” request to be completed by your doctor. This is normally needed when the treatment is not listed on your insurance company’s formulary list. Your doctor has to submit additional information to show medical necessity, explaining why treatments on the formulary are not appropriate.
Not Covered
 Some medications and many of the devices are not covered by insurance at all. At times it is possible to appeal this with a medical necessity letter from your doctor and a long history of failed alternative treatments. The companies which offer medical devices for migraine are currently working on insurance coverage for patients.
Some medications and many of the devices are not covered by insurance at all. At times it is possible to appeal this with a medical necessity letter from your doctor and a long history of failed alternative treatments. The companies which offer medical devices for migraine are currently working on insurance coverage for patients.
Advocating for yourself is crucial in navigating this insurance process, otherwise, treatment approvals can take longer than necessary or even simply not happen. It helps to stay on top of the status of any treatment your doctor has prescribed for you. Here are some options for self-advocacy:
- Talk with your pharmacy to make sure that they have communicated any denial to your doctor's office
- Stay in touch with your doctor's office regularly to get status updates
- Call your insurance company directly to initiate an appeal after a denial
- Ask other people with migraine for advice on how to navigate the process
- Use the HMPF Complaint Guide to file a formal grievance against your insurance company
- Join with other patients and providers to advocate for change by using our Insurance Advocacy Toolkit
- If all self-advocacy attempts fail, there are patient advocacy organizations such as the Patient Advocate Foundation which may be able to help
Learn, and Take Action!
Click on the images below to learn more about barriers to access imposed by insurance companies and what you can do. Participate in the advocacy campaign launched by Migraine Meanderings and The Headache & Migraine Policy Forum this April!