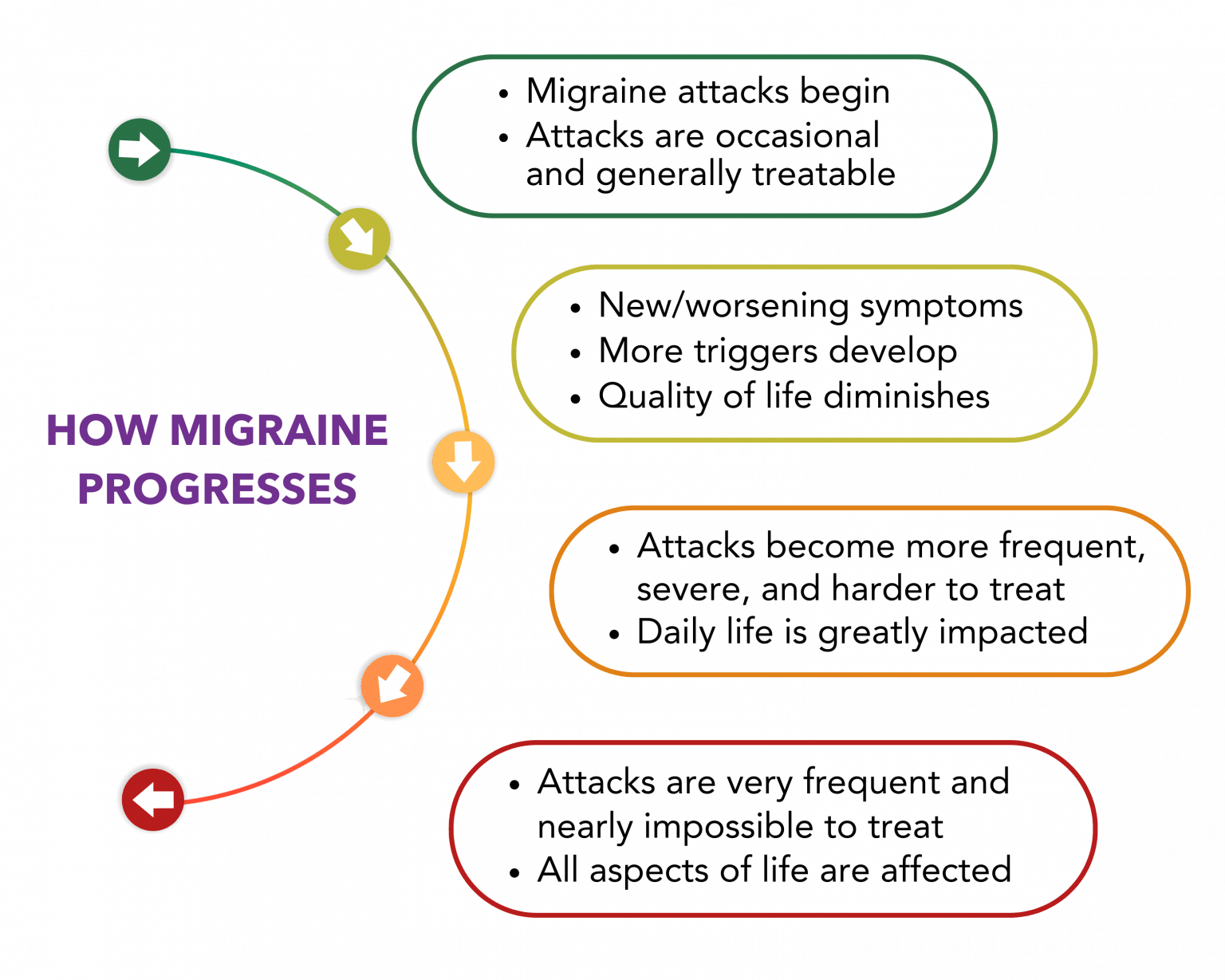
Did you know, without effective treatment migraine disease can get worse?
- We can take steps to help prevent and reverse migraine progression, also known as chronification.
- Appropriate, timely, and effective treatments are key to minimizing the risk of disease progression.
- As migraine symptoms, frequency of attacks, and response to treatment changes, our treatment plan needs to change too.
You deserve better NOW!

Watch the Video!
When migraine progresses, attacks become more frequent & severe, last longer, & are harder to treat. This video looks at the stories of 4 patients who live with migraine, & how it has impacted their lives. Their stories, unfortunately, are like many others. If your migraine has become worse, talk to your doctor about updating your migraine treatment plan!
You Deserve Better NOW!
Optimizing migraine management helps reduce the risk of chronification and the impact on your quality of life.
Explore Migraine
Treatment Options
Find a Certified
Headache Specialist
"I wish I had known that migraine could chronify; I wouldn’t have insisted on ‘pushing through’ so often and would have taken this disease more seriously!"
—Shoshana
"If I had known early on in my life that migraine would become so debilitating and impact my life so negatively, I would have sought treatment sooner in preparation for the possibility of a more complicated lifestyle."
—Aaron
"Migraine is an ever-changing presence in my life. I’m so grateful for the work of advocacy organizations who have taught me so much about how to manage this unfortunate disease and reclaim my quality of life."
—Jessica
"I wish I had known how to advocate for myself at an earlier age, and had not felt I was weak asking for medication to help with the pain."
—Angel

Watch the Video!
Dr. Gottschalk discusses how migraine is progressive, and explains how to reduce the risks of disease chronification.
A Migraine Action Plan is "the single most important thing that somebody should come away with from a consultation with a headache specialist or whoever's treating your migraine." Dr. Christopher Gottschalk
Migraine Progression FAQs
Answers from Dr. Gottschalk
General Questions
Chronification Risks and Causes
Signs of Progression
Prevention and Disruption
About Dr. Gottschalk

Christopher H. Gottschalk is currently Director of the Yale Headache & Facial Pain program and Chief of the section of General Neurology. He was UCNS board-certified in Headache Medicine in 2012 and was made Fellow, AHS, in 2014, where he is active in curriculum development, working to establish milestones for Headache Medicine knowledge and practice.
Dr. Gottschalk’s primary research interest is in education—from neurology trainees and Primary Care physicians to the general public—regarding the facts of headache disorders and the fictions that interfere with their recognition and treatment.