Blog Content Medically reviewed by Christopher Gottschalk, MD.
Thanks to our industry partner, Lundbeck, for sponsoring this educational project.
Did you know that migraine is a progressive disease? Maybe this is the first time you have heard this. Or maybe you’ve heard rumors, but have dismissed them as only applying to people who are really sick with migraine, and think, “that’s not me.” Unfortunately, it is true, but some steps can be taken to help disrupt the progression of migraine. Realistically, too many people with migraine are not taken seriously, not only in society in general, but also in the healthcare system. People who live with migraine deserve better!
If you live with migraine, some steps can be taken to help address the chronification risk. Ask yourself, “Am I having more migraine attacks than before?” “Are my symptoms more severe and/or harder to treat?” “Is my quality of life being impacted more?” If the answer to any of those questions is “yes,” that may indicate chronification – disease progression. It’s time to talk with your headache doctor!
Migraine is a progressive, chronic neurological disease. As it progresses, multiple things may start happening: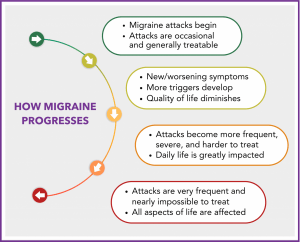
- Attack frequency can increase
- Attack severity can get worse
- Length of individual attacks may increase
- Symptoms may change or even multiply
- You may become more sensitive to attack triggers
- You may become less responsive to migraine treatments
Do I Have Episodic or Chronic Migraine, and Does That Matter?
It’s important to know what type of migraine you have – specifically, whether it is episodic or chronic. Having a diagnosis of “chronic migraine” doesn’t mean you have had it for a long time. A chronic migraine diagnosis means you have 15+ headache days a month for at least 3 months, with the features (symptoms) of migraine on at least 8 of those days.
Getting an accurate diagnosis from a doctor, preferably a certified headache specialist or general neurologist, is key. This will help you determine the best Migraine Action Plan (MAP) and better see if the disease worsens over time.
- Episodic migraine attacks are classified as less than 15 headache days a month. A headache day is any day with attack symptoms. Episodic migraine can progress from occasional to low-frequency episodic, from low-frequency to high-frequency episodic, and then to chronic migraine.
- Chronic migraine is classified as 15 or more headache days per month for at least 3 months, with migraine features (symptoms) on at least 8 days per month. A migraine feature can be throbbing pain on one or both sides of the head, nausea, and sensitivity to light, sound, and smell.
In addition to the changes listed above (frequency, severity, etc.), you may also be experiencing allodynia. This often-challenging symptom means that you are becoming hypersensitive to things that should not usually feel painful. Allodynia may be present during and/or in between migraine attacks, and can present in many forms. For example, you may feel pain when brushing your hair, wearing a hat, putting your hair in a ponytail, or even just touching your head! It could also be an increased sensitivity when touching something cold that would not usually feel painful, or even a light touch from someone close to you.
Why Does Migraine Progress (Chronify)?
Figuring out how or why, or even if, your migraine disease is progressing, also known as “chronifying,” can be challenging. Migraine attacks have a reputation for being somewhat erratic and hard to pin down. You may have a good month followed by a bad month, and then back to good again. However, if you carefully monitor your attacks and symptoms over a period of time, you may be able to start to recognize the impact of disease changes. Factors associated with a risk of migraine progression include:
- Additional comorbidities: Having additional chronic (comorbid) conditions, as well as migraine, is one risk factor for chronification. Common comorbid conditions include depression, anxiety, other pain disorders, autoimmune disease, asthma, sleep apnea, and many more. If you have any of these conditions, let your headache doctor know so they can better understand your migraine chronification risk.
- Not treating acute attacks appropriately: When migraine attacks are not treated quickly and effectively, the pain may increase or last longer. When you have more pain, your central nervous system becomes more sensitive to that pain, resulting in migraine being triggered more easily(1). This sensitivity, often known as central sensitization, can result in symptoms such as allodynia. This is where it is crucial to have and to follow a personalized Migraine Action Plan. It’s essential to start treatment at the first sign of attack symptoms, and to know that “pushing through,” or “taking the edge off,” increases your risk for chronification.
The MTOQ(2) is a 4-question form that helps evaluate the efficacy of someone’s acute medications:
-
- Question 1: When you take your acute migraine medicine, are you pain-free in two hours or less?
- Question 2: Does your medication enable you to remain pain-free for at least the next 24 hours?
- Question 3: Does your current acute treatment mean you’re comfortable planning normal activities?
- Question 4: After taking your acute medication, do you feel in control of your migraine enough so that you feel you can return to normal function?
Answering the MTOQ and sharing the results with your doctor can be really helpful. Armed with that information, you can better partner with your doctor to develop a more effective treatment plan and help disrupt potential migraine progression.
- Medication Adaptation Headaches: Also known as rebound headaches, medication overuse headaches, or “MOH.” The theory is that MOH happens when too much acute migraine medication is used. However, some headache specialists believe that MOH is overdiagnosed, and hinders addressing the root problem, which is chronification. MOH is considered a secondary headache, while migraine is considered the primary headache. Identifying the difference between the two will help determine the type of headache attacks you are having. An over-focus on MOH can hinder the treatment of migraine and the creation of an effective, personalized Migraine Action Plan. If you are frequently taking acute medications to relieve migraine attacks, it may be time to add a new or additional preventive treatment to your migraine toolbox.
- “One and done” approach: Migraine prevention and acute treatment are often most successful when there is a toolbox approach to disease management. Preventive treatments such as medications, medical devices, and non-pharmacologic options such as acupuncture or biofeedback, may help to reduce the number of migraine and headache days you have each month.
When combined rather than used alone, specific acute treatment options can often stop an attack in its tracks or shorten its length and severity. Some treatments—e.g., non-oral medications—may be more effective than a pill form of the same medication, particularly if you have nausea, vomiting, or gastroparesis during attacks. The route of administration or “formulation” matters. This is why it is crucial to have a personalized Migraine Action Plan that you create together with your headache doctor, and which adapts as your migraine disease changes. Sadly, the “one and done” approach, often used for migraine attacks, is rarely effective over time.
- Outside factors: Daily stress, traumatic events, a neck injury, or even heavy use of caffeine for some people, can also contribute to the progression of migraine. While we often cannot prevent what happens to us, we can learn to manage the consequences better. Adding things such as lifestyle adjustments, meditation and mindfulness, biofeedback, or tai chi to your migraine toolbox may help with frequent migraine attacks and the associated symptoms.
- Severe nausea: Interestingly, if you have frequent, severe nausea with your attacks, that is one indicator that your attacks are bad and are likely to get worse. This is something that patients can keep an eye out for, realizing that if this starts to happen, then they may need to be more proactive about disease management.
Is Migraine Chronification Preventable?
Yes! Episodic migraine can escalate and become chronic very quickly. It’s never too soon to create a management plan to prevent migraine attacks from worsening. Here are some ways to help prevent the process of migraine chronification, or at least reduce the risk:
to help prevent the process of migraine chronification, or at least reduce the risk:
- Learn all you can: Visit our new migraine chronification / progression website page, which includes helpful resources, FAQs, and an incredibly informative video recording with a certified headache specialist, Dr Christopher Gottschalk, about this topic!
- Use a Migraine Action Plan to guide your treatment: A Migraine Action Plan is a written plan you develop with your doctor to manage migraine and headache symptoms outside the doctor’s office. The MAP includes recommended preventive and acute treatment, and when it is appropriate to call your doctor or go to the ER. It explains which treatments to start and when, including FDA-cleared medical devices, at-home therapies, medications, and more.
The MAP details what to do if your first acute treatment doesn’t work for an attack, and provides guidelines on when to call your doctor or seek immediate medical care. A Migraine Action Plan takes much of the guesswork out of treating your migraine and other headache symptoms and helps empower YOU, the patient. In a recent webinar on this topic, Dr. Gottschalk stated, “A Migraine Action Plan is the single most important thing that somebody should come away with from a consultation with a headache specialist or whoever’s treating your migraine.”(3)
- Treat acute symptoms quickly: Start acute treatment options as directed by your doctor at the first sign of symptoms. Remember, the longer you stay in pain, the more likely you are to develop central sensitization, resulting in more pain. If possible, don’t push through the pain unless absolutely necessary. Instead, when you have a migraine, stop, treat, and rest if at all possible. This may not only help relieve acute symptoms more quickly but also may help reduce the risk of chronification.
- Add preventive treatments when needed: If you are experiencing 4 or more migraine days a month, or even two attacks that rob you of all or most of a day, talk with your doctor about possibly adding a preventive treatment to your MAP. If your current preventive treatment isn’t effectively reducing the frequency and severity of attacks, talk with your doctor about possibly adding another one or making a change.
- Add acute treatments if appropriate: If your acute medication or other treatment is not effectively stopping your migraine attacks, talk with your doctor about your options. A toolbox approach may work best to help stop attacks, and it could include a combination of one or more medications, a medical device, lying down in a dark, quiet room, and other tools such as an ice hat or dark glasses.
Visit our new Disrupting the Progression of Migraine resource for more information. Click Here to Learn More!
Can Chronic Migraine Be Reversed?
This is the million-dollar question that patients so often ask. The truth is, it’s difficult to reverse migraine progression; however, it is not impossible! “The biggest problem we face is that people think whatever they have is as good as it gets. And yet, we know that there are actually really effective tools out there that are being underutilized, and that people don’t even know what the definition of a good response is. So inform yourselves. It is possible to get better!” Dr. Christopher Gottschalk(4)
Here are ten steps to help increase the chances of disrupting migraine chronification:
- Create a Migraine Action Plan with your doctor
- Treat acute symptoms quickly
- Reduce attack frequency with preventive treatments
- Manage comorbid conditions
- Identify and reduce exposure to migraine attack triggers
- Make helpful lifestyle adjustments
- Have a toolbox approach to disease management
- Connect with others who live with migraine for ideas, tips and support
- Educate yourself with evidence-based information
- Don’t give up hope!
Summary
It is essential to realize that migraine, whether low-frequency episodic, high-frequency episodic, or chronic, is a progressive neurological disease. It is also crucial to recognize that migraine impacts people differently, and there is no “one size fits all” treatment. Unfortunately, partly due to the global shortage of certified headache specialists and the lack of migraine and headache disorder education in medical schools, patients as a group need to be actively involved in managing the disease we live with. The first key step is accurate diagnosis, which is just the beginning. Diagnosis must be followed by disease-appropriate, effective, and tolerable treatment as soon as possible.
Most of all, remember – there is always hope, and you deserve better NOW! As a patient advocacy organization, we have the privilege of hearing patients’ stories all the time. Some of those stories are literally life-changing! We’d love to hear your story too, and support you in your migraine journey. Visit our new “Migraine Progression” website page HERE to identify strategies to disrupt migraine progression. Let us know what you think!
Let Us Know!
Have your migraine attacks changed over the years? Have the attacks become more frequent, severe, and/or harder to treat? Have you been able to go from chronic migraine back to episodic, or high-frequency episodic to low-frequency episodic?
Disclaimer
Please note that this blog post is for informational purposes only and is not intended to provide medical or treatment advice. If you have any questions about your individual care, please reach out to your healthcare provider.
Citations & Sources
- Suzuki K, Suzuki S, Shiina T, Kobayashi S, Hirata K. Central Sensitization in Migraine: A Narrative Review. J Pain Res. 2022 Sep 7;15:2673-2682. doi: 10.2147/JPR.S329280. PMID: 36101891; PMCID: PMC9464439.
- Dr. Richard Lipton, https://www.mdcalc.com/calc/10496/migraine-treatment-optimization-questionnaire-mtoq-4
- Dr. Christopher Gottschalk, “Disrupting the Impact of Migraine: A Progressive Disease” https://migrainemeanderings.com/migraine-toolbox/migraine-progression
- Dr. Christopher Gottschalk, “Disrupting the Impact of Migraine: A Progressive Disease” https://youtu.be/Qb4TwNyTwZs?si=9p4AmhskZX8DUANs
Many thanks to our industry partner, Lundbeck, for supporting this educational project.